The surprising truth about sugar. Here’s everything you need to know about what it does to your body.

Is sugar “good”?
Is sugar “bad”?
It’s hard to know for sure these days.
Which is interesting because…
Sugar is a fundamental molecule in biology.
Human bodies need sugar.
Sugar makes up the backbone of our DNA. Helps power our cells. Helps store energy for later. Plants convert sunlight into sugar. We convert sugar into fuel.
Molecules like glucose and fructose (just two of the many types of sugar) are so basic to our biological needs, even bacteria love them.
Indeed, sugar’s the breakfast of champions, chemically speaking.
Yet, somewhere along the way, sugar became the bad guy.
Why did we start hating on sugar?
When did we start wanting to purge it from our bodies?
Why do some of us fear it so much?
At this point… do we just need a little relationship counseling?
Or is it a toxic relationship?
Is it time to part ways?
The truth is, this is a difficult conversation to have because…
Almost all of us are emotionally invested in our position on sugar.
Talking about it brings up a lot of controversy and intense debate, even among scientists who are supposed to be “objective”.
So why not step back and take a fresh look?
In this article, we’ll explore five key questions about sugar:
- Does sugar cause obesity?
- Does sugar cause us to gain weight / fat?
- Does sugar cause diabetes?
- Does sugar cause cardiovascular disease?
- How much sugar is OK to eat?
Yes, we’re biased too.
At Precision Nutrition, we generally consider ourselves ‘nutritional agnostics’. (Case in point: our view on the absolute best diet.)
We help people become their healthiest, fittest, strongest selves—in a way that works for their unique lives and bodies.
In our work with over 100,000 clients clients, we’ve learned a few things…
… that one size doesn’t fit all,
… that an all-or-nothing approach doesn’t work for most people,
… that fitness and health habits should be doable on your worst day, not just your best.
So here’s our bias in this article.
We follow the complexities of nutrition evidence as best we can, always interpreting them through the lens of:
- How does practice X or Y work for us, for the clients we coach, and for the fitness professionals we certify?
- Does said practice help us make our food choices wiser, saner, and simpler?
- Does it address individual differences between people?
- (And if not, how can we help adapt each person’s diet to match their unique needs?)
You can ask yourself these same questions as you go through the article. And, of course, feel free to come to your own conclusions.
But first, let’s get to know our sugars.
What is sugar?
Most of us think of “sugar” as the white stuff we put in coffee, or maybe what makes up 90% of those colored marshmallow cereals.
However, “sugar” is actually a group of molecules that share a similar structure. So we might actually call them “sugars”, plural.
This group includes lots of members such as:
- glucose
- fructose
- sucrose, aka table sugar (which is glucose + fructose)
- maltose (which is glucose + glucose)
- galactose
- lactose (galactose + glucose, found in dairy)
And so on.
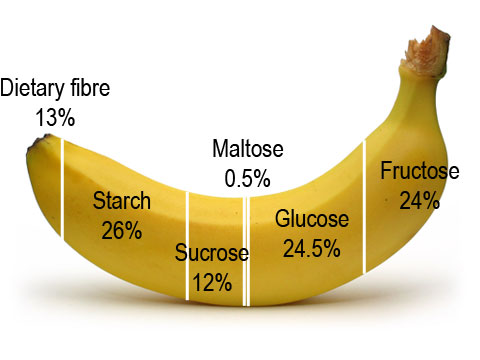
Sugars naturally occur in biology and in most foods (even if just in trace amounts). For example, here’s what the breakdown of sugars looks like in a banana:
There is, of course, much more sugar in processed and refined foods than in less-processed and unrefined foods.
(We’ll come back to this important point in a moment.)
Sugars live under the larger umbrella of “carbohydrates”.
Along with the sweet stuff, this macronutrient group also includes:
- starches (like in potatoes or rice),
- fiber (like the husks of whole grains), and
- structural building blocks like chitin (which makes up the shells of crustaceans) or cellulose (which makes up things like the trunks of trees).
The more complex the molecule, the slower it digests.
- Sugars, which are simpler, digest more quickly.
- Starches and fiber, which are bigger, more complicated molecules, digest more slowly, if at all. (This is why eating more fiber can help us feel fuller, longer.)
Most carbohydrates are actually broken down into simpler sugars once they’re digested.
Other carbohydrates (such as insoluble fiber) don’t really get broken down nor absorbed fully, although our intestinal bacteria often love munching on them.
So: Sugars are a type of carbohydrate, but not all carbohydrates are sugars. And some carbohydrates break down quickly/easily into sugars. Others don’t.
This point is important to understand, because it tells us that not all carbohydrates do exactly the same things in our bodies.
Evolution has helpfully given us the ability to “taste” sugar.
Sugar-type molecules react with receptors on our tongue, which then tell our brain “OM NOM NOM DELICIOUS!”
Sugar tastes good to us, because in nature, sweet foods like fruits are often full of good stuff like vitamins, minerals, and energy.
But we differ in our physiology and behavior.
In all things, humans are diverse and variable.
Some of us like and seek out sugar more than others. This may be genetic. Or we may have learned it as we grew up. Or both.
For example, some of us like sugar in small doses; we can only eat a little before pushing the dessert plate away. While others like it a lot; the more we eat the more we want. The idea of “too much sugar” doesn’t compute.
Likewise, some of our bodies seem better suited to sugar than others.
For example, some of us can eat sugar all day long and feel fine. While others can only tolerate a little bit before our pancreas (which secretes insulin, a hormone that helps sugar get into the cells) tells us to knock it off.
In general, most of us like at least some sweetness.
When we’re young, we tend to like sweetness more and avoid bitter foods more. Yet each person’s response to sugar and sweet taste is unique.
With that said, let’s get back to the questions at hand. Starting with…
Question #1:
Does sugar cause obesity?
The term “obese” (or “overweight”) is, like sugar, a contentious thing. In this article we’ll use it just for the purpose of discussion, so bear with us.
The World Health Organization defines “obese” as having a Body Mass Index higher than 30. Of course, some fit athletes (like heavyweight boxers or rugby players) might have a higher BMI but still have a low body fat percentage.
However, for most folks, having a BMI higher than 30 signifies that they have a higher-than-average level of body fat.
(Indeed, some studies that correlate BMI with body fat testing suggest that BMI may even under-estimate how much body fat a person has.)
When it comes to obesity, there have always been people who are heavier, and/or who have more body fat, than most other folks like them.
However, over the last several decades, “average people” in industrialized countries have gotten heavier, bigger, and gained more body fat fairly rapidly.
It’s now statistically “normal”.
Although this shift is happening worldwide, and there are differences by ethnic group and socioeconomic class, it’s particularly noticeable as a general trend in the United States.
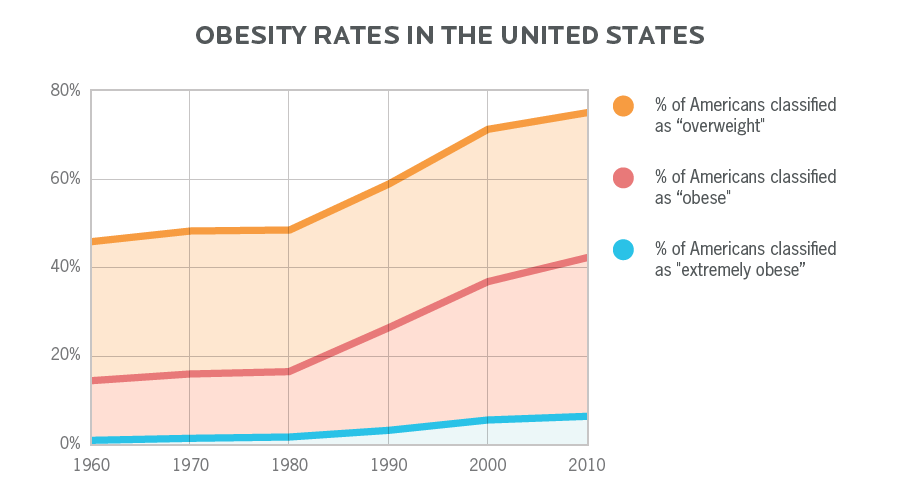
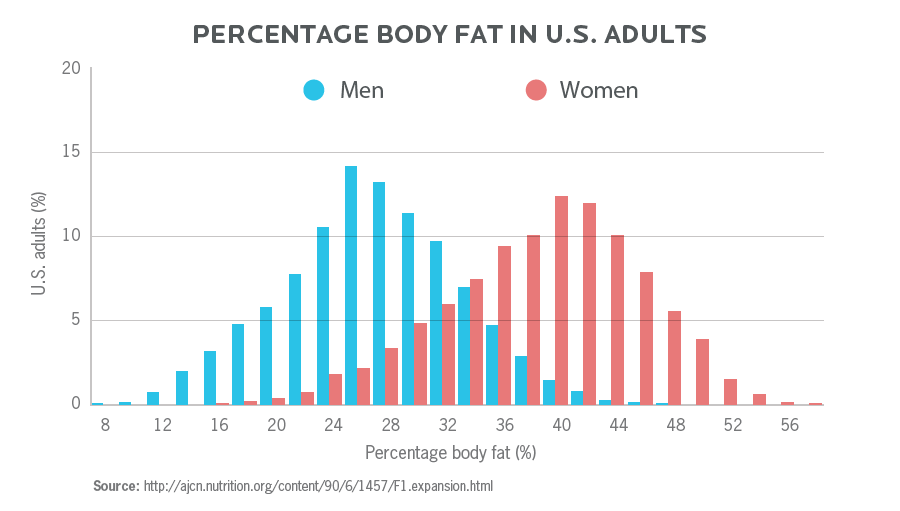
Along with body weights, we can look at changes in body fat percentage and overall fitness levels. Here, we also see that over time, body fat percentage has gone up, and fitness levels have gone down.
Currently in the United States, the average body fat percentage for men is around 28%, and the average for women is around 40%.
For comparison:
- In general, 11-22% for men, and between 22-33% body fat for women, is considered a “healthy” range.
- Lower than that is still “healthy” (to a point), but generally considered “athletic” or “lean”.
Does increased sugar consumption explain body weight trends?
Could sugar be responsible for changing body weights and body compositions in industrialized countries?
By reviewing data from the USDA Economic Research Service, National Health and Nutrition Examination Surveys (NHANES), as well as Food Frequency Questionnaires from the long-running Framingham Heart Study, we can track food intake from multiple angles. These varying streams of data all show fairly consistent trends.
They tell us that, since 1980, Americans:
-
Continued to eat the same total amount of fat.
(Though they generally ate less naturally-occurring fats, like in whole fat dairy, and ate more added fats, like oils.)
-
Ate more carbohydrates.
(Especially refined ones that included added sugars.)
So, as a percent of total calories consumed, fat dropped. But we didn’t end up eating less fat. We just added more sugar and other carbs on top of the fat we were already eating.
This added up to approximately 200-400 extra calories per day.
In terms of calories, that’s like eating an extra McDonald’s hamburger or a double cheeseburger, on top of your existing meals, every day.
Whether those calories came from sugar is probably irrelevant.
This increased energy intake alone, combined with decreasing rates of daily physical activity, is probably enough to explain people getting heavier.
Yes, but how might sugar play a role?
We can’t say that sugar specifically was the culprit behind the obesity surge for everyone. (Remember, humans vary.)
But our increased sugar consumption does seem to correlate with continued obesity levels… up until recently.
For about four hundred years, human beings have been enjoying more and more sugar.
Once Europeans discovered tropical trading routes and set up cheap slave labor economies to raise sugar cane, sugar became more and more available to the average person.
Indeed, sugar quickly became the food of the poor.
(It was said that the entire working class of the British Isles lived on jam and sugared tea during the Industrial Revolution.)
As a prime colonial power, the British once claimed the title of biggest sugar consumers. Per year, the average Brit consumed:
- 4 lbs (1.8 kg) in 1704.
- 18 lbs (8.2 kg) in 1800.
- 90 lbs (40.8 kg) in 1901.
However, once they got rolling as a country, Americans weren’t far behind. Per year, the average American consumed:
- 6 lbs (2.7 kg) of sugar in 1822.
- 40 lbs (18.1 kg) in 1900.
- 90 lbs (40.8 kg) by the 1920s.
- There was a subsequent drop due to the Great Depression & World War II.
- 90 lbs per person again by the 1980s.
Then they really took off: By 1999, the US reached peak sugar consumption of nearly 108 lbs (49 kg) of sugar per person per year.
Between 1980-1999 Americans ate more sugar. And obesity rates got higher.
But then something changed: Our sugar consumption actually started to decrease.
Interestingly, since 1999 through 2013 (most recent data available) intake of added sugar has actually declined by 18% (or as much as 22%, depending on the data).
This drop has brought Americans’ current added sugar intake back down to 1987 levels.
And during this time, total carbohydrate intake has dropped as well. (Makes sense, as this was the dawn of the low-carb phenomenon.)
Nevertheless, though sugar and carb intake have declined over those 14 years, adult obesity has continued to climb—from 31% of the American population in 1999 to 38% as of 2013.
(Diabetes diagnoses have continued to climb as well, which we’ll address in a moment.)

So, despite lowering sugar intake by nearly 20% over a 14 year period, obesity (and diabetes) rates have continued to climb.
Along with sex, ethnic, and socioeconomic differences in obesity rates, this suggests that changing body sizes and compositions is probably a complex, multi-factored phenomenon.
Bottom line here: No single thing—including sugar—causes obesity.
Many factors work together to contribute to a consistent energy (calorie) surplus, which ultimately leads to fat gain. One of those things is often sugar, but not always, and not alone.
Question #2:
Does sugar cause us to gain weight / fat?
So, we can’t unequivocally blame sugar for increased obesity rates.
But many of us are still wondering whether sugar is a gateway to fat gain.
It seems logical. Carb and sugar consumption are the main drivers of insulin release. Insulin’s job is to help store nutrients, including fat.
Therefore, it seems obvious. Carbs and sugar cause fat gain, right?
Once again, our scientist friends reveal that it’s a bit more complicated than that. Let’s take a look at a couple of studies that explore this question.
Study 1: How do carbs, sugar, and/or insulin release affect body fat?
In 2015, a small pilot study was conducted by Dr. Kevin Hall to investigate the carb/sugar/insulin model of obesity.
What happens if we keep calories and protein the same, but play with dietary sugar and fat levels?
Here’s how the study worked.
- 19 participants had to live in a metabolic ward, where the researchers controlled virtually everything about how they lived, what they ate, etc.
- The participants tried both lower carbohydrate (LC) and lower fat (LF) diets.
- They followed each diet for two weeks, separated by a 2-4 week period during which they returned to normal eating.
- All participants spent the first five days of either the low-carb or low-fat diets following a baseline plan of 50% carbs, 35% fat, and 15% protein. This was done so that all participants started on an even playing field with an intake that virtually matches what the average American eats.
- Each participant had to exercise on a treadmill for one hour every day for the full two weeks, to make sure physical activity levels were consistent and equal.
- After the first five days, both groups had their calories reduced by 30% from the baseline diet (1918 calories vs 2740 calories). They then ate the lower calorie diet for six days.
- With both diets, energy intake (i.e. calories) and protein were kept the same. Only carbs and fat went up or down.
Lower carbohydrate:
- 101 g protein (21% of cals).
- 108 g fat (50% of cals).
- 140 g carbohydrate (29% of cals).
Lower fat:
- 105 g protein (21% of calories).
- 17 g of fat (8% of calories).
- 352 g carbohydrate (71% of calories).
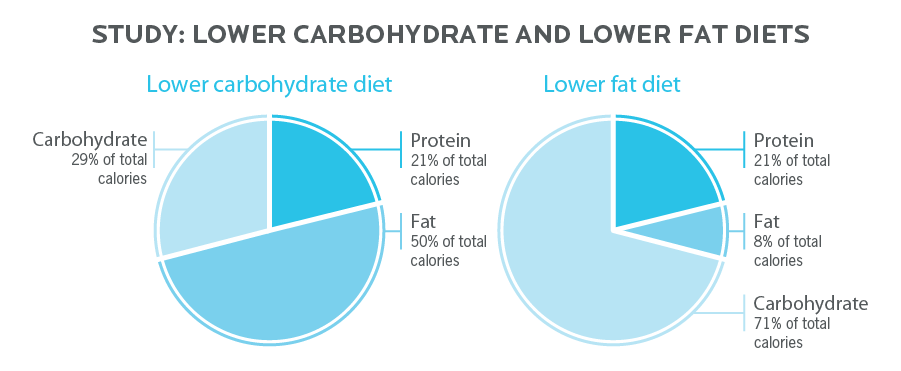
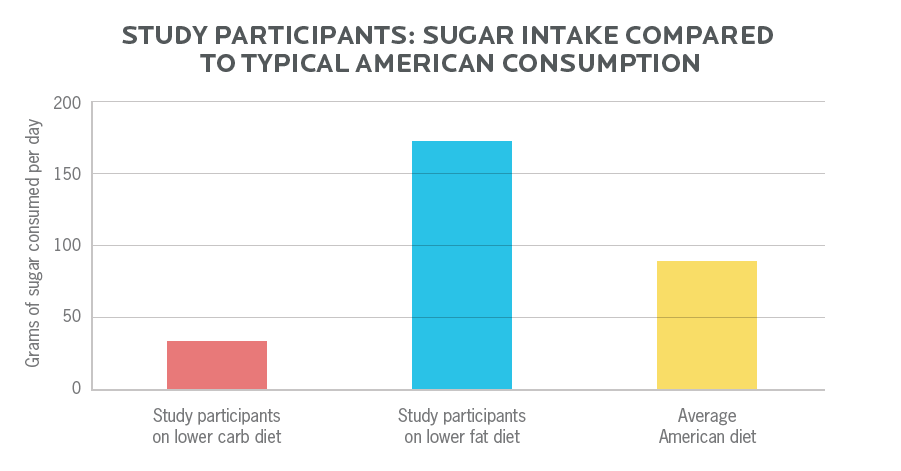
Let’s take a closer look at how much the study participants actually ate.
On the lower carbohydrate diet:
- Of their carbohydrates, 37 g was sugar. This means that 8% of all calories were coming from sugar.
- This is much less than the average American eats.
On the lower fat diet:
- Of their carbohydrates, 170 g was sugar. This means that 35% of all their calories were coming from sugar. That is a lot of sugar.
So what happened?
Insulin production:
- On the Lower Carbohydrate diet, people produced 22% less insulin throughout the day.
- The Lower Fat diet didn’t change insulin output at all, since it had the same total carbs, and even slightly more sugar than the baseline diet.
Body weight:
- People on the Lower Carbohydrate diet lost 4 lbs (1.81 kg) of body weight, and 1.16 lbs (0.53 kg) of body fat.
- People on the Lower Fat diet lost 3 lbs (1.36 kg) of body weight, which included 1.29 lbs (0.59 kg) of body fat.
Note that body weight loss doesn’t necessarily equal body fat loss.
We can also lose body weight from losing glycogen, water, and/or body protein—and that’s exactly what happened to the people on the Lower Carb diet.
They lost more overall body weight, but actually lost less fat. (Though a difference of 0.13 lbs is irrelevant in the big picture. Who would notice that?)
Meanwhile, the folks on the Lower Fat diet lost more body fat but less total weight because their body was busy burning fat (rather than glycogen or lean body mass) to meet its calorie needs.
After these results were in, the researchers then ran validated mathematical models that showed over longer periods of time (say, longer than 6 months), the fat loss between the two groups would be roughly equal.
In other words, there was no particular physiological advantage to either diet in terms of body weight, nor body fat loss, over the longer term.
Study 2: Fine, let’s go lower.
For this second study, the game got hardcore: Drop the carbs and sugar much lower for the Lower Carbohydrate group, just to make sure the minimal differences found in the first study hadn’t been because the carbs and sugar weren’t low enough.
Here’s how this second study worked:
- 17 overweight or obese people participated.
- First, they followed a high-carb but calorically-restricted baseline diet for 4 weeks (with 25% of calories from sugar).
- Then, they spent 4 weeks on a very-low-carb ketogenic diet (with 2% of calories from sugar), with equal calories to the baseline diet.
So what happened?
The researchers found that everyone lost weight and fat throughout the study.
However, when subjects switched from the high-carb, 25%-sugar baseline diet to the ketogenic, 2%-sugar diet, fat loss actually slowed down for the first few weeks.
Much like the previous study, this happened because as people’s bodies adapted to the ketogenic diet, they were more likely to break down fat-free mass and protein stores (e.g. muscle).
Thus:
- Weight loss went faster during the ketogenic phase, thanks to losing glycogen and water.
- But body fat loss was actually less during this phase (though not tremendously so, and it likely wouldn’t make any significant difference over time).
Overall, the researchers stated that based on the current evidence, as well as their validated mathematical models, long-term body fat loss would likely be very similar between the high sugar (high-carb) diet and the low sugar (low-carb) diet.
In other words, the amount of sugar didn’t seem to influence the results.
In the end, these, plus other studies, seem to support the idea that:
Sugar, carbohydrate intake, and/or insulin alone probably aren’t the main drivers of weight gain.
Other research comparing low-carb diets to low-fat diets has found similar results. The same results have also been found with:
- Meta-analyses: Big reviews of other studies. These types of data are considered among the most robust as they explore a lot of experiments from a much broader perspective, pulling in evidence from dozens or even hundreds of studies to try to draw conclusions.
- Systematic reviews: Methodologically rigorous comparisons and critical analyses of other studies. These type of reviews are also considered useful, because they take a skeptical perspective, looking for errors.
There have been at least 20 controlled in-patient feeding studies where protein and calories are kept equal, but carbs are varied from 20% to 75% of total calories (and sugar intakes ranged significantly as well).
Of all these studies, none of them found any truly significant differences in body fat levels when people were eating either high carb (and high sugar) or low carb (and low sugar) diets.
In other words, as long as protein and calories were equal, the amount of sugar people ate didn’t make a difference.
There have been at least 12 other systematic reviews and meta-analyses published over the past 10+ years on long-term low-carb diets (which are invariably also low-sugar diets).
Of these 12 reviews:
- 3 were in favor of low-carb
- 3 were in favor of non-low-carb comparisons (e.g. low fat, Mediterranean, vegan, low glycemic index, etc.)
- 6 were neutral, meaning they concluded that various approaches can be equally valid and effective.
Yes, but how might sugar play a role?
Sweet foods may increase energy intake.
In 2013, a review commissioned by the World Health Organization investigated how sugar affected fat gain.
It found that increasing sugar intake can increase body weight, and lowering sugar intake can decrease body weight… but only by changing energy balance, not by any physiological or metabolic effect of sugar itself.
In other words, if we eat more sugary foods, we might be eating more energy (i.e. calories) overall.
Sweet foods are often processed and highly palatable.
This is especially true because most high-sugar foods are refined, tasty, and hard to stop eating. We digest and absorb the energy they contain quickly and easily, they overstimulate the reward/pleasure centers in our brain, and we tend to overeat them.
Plus, hidden sugars in processed foods (like yogurt, granola, juice) or even so-called “health foods” / “fitness foods” can add up fast without us even realizing.
These foods and our brain’s response to them, not the sugar by itself, can often lead to overconsumption.
So the sugar itself may be less of a culprit than the fact that many of us just can’t quit at just one gummi bear or sip of soda.
What else is going on, besides sugar consumption?
Most of our clients who struggle with their weight, body fat, eating habits, and health tell us: It’s not just about the food. There are many factors involved: stress, sleep, metabolic health, lifestyle, social environment, and so forth.
Sugar alone does not explain the complexity of our bodies’ health, function, fat percentage, nor weight. Metabolism is complicated.
And, as always, remember that people vary in response to particular diets.
Some people do better with higher carbohydrates and lower fats. Some do better the other way round.
This is likely due to genetic differences, individual satiety differences from fats vs carbs, personal preferences, and possibly even differences in the bacterial populations in our GI tracts.
The above studies don’t provide hard and fast rules that will always apply to everyone.
This is especially true given that many study populations were small and probably similar in terms of age, sex, ethnicity, and other important factors that can affect our physiological response to a given diet.
But they do indicate that sugar is not some kind of unusually evil substance that causes weight gain or prevents fat loss.
Question #3:
Does sugar cause diabetes?
Diabetes is a disease where we can’t properly regulate the sugar in our blood.
It seems logical, then, that eating more sugar might increase our risk for diabetes, particularly Type 2 diabetes, also known as adult-onset diabetes.
Unlike Type 1 diabetes, which typically starts in childhood and is considered an autoimmune disease (in which our own bodies attack healthy cells of our pancreas, which normally produces insulin), Type 2 diabetes typically starts later in life and (among other factors) is linked to long-term food and exercise behaviors.
Type 2 diabetes generally starts with insulin resistance, or impaired glucose control.
This means that over time, insulin is less and less able to do its job of moving glucose into our cells for safe storage. Your doctor might test this with various blood tests, such as an A1c test, which measures how much sugar is being carried around on hemoglobin, a blood protein.
Type 2 diabetes (as well as other metabolic diseases) are also related to how much fat we have in our livers and in or around other organs (such as our hearts and kidneys).
There does seem to be a link between how much refined sugar we eat and insulin resistance. Eating too much sugar can also increase fat accumulation in the liver.
For example, a recent study found that for every 150 calorie increase in daily sugar intake (essentially a 12 oz soda, or ~37 g) corresponded with a 1.1% increased risk for diabetes.
Other factors shape our disease risk, too.
That risk above might sound scary, but it’s important to keep it in perspective.
Other research has shown that losing 7% body weight and doing about 20 minutes of daily physical activity decreased diabetes risk by 58%.
And many other studies have corroborated those findings, telling us that losing a little weight / fat and doing a little more exercise, consistently, will significantly lower our diabetes risk.
In fact, a recent meta-analysis provided some compelling information on diabetes risk:
- ~60-90% of Type 2 diabetes is related to obesity or weight gain, not sugar intake.
- Having a significant amount of excess body fat / weight can increase diabetes risk by 90 times.
- If people who are in the obese category lose about 10% of their initial body weight, they dramatically improve their blood glucose control.
- Weight management (not sugar reduction) appears to be the most important therapeutic target for most individuals with Type 2 diabetes.
This makes sense if we understand how adipose (fat) tissue works: It’s a biologically active tissue that secretes hormones and other cell signals.
If we have too much of it, adipose tissue can disrupt metabolic health, including how we regulate and store blood sugar.
Does fructose contribute?
Some researchers have suggested that fructose, a particular type of simple sugar (aka monosaccharide) found in fruit as well as many processed foods, might play a special role in diabetes.
We know that fructose is digested, absorbed, and used in specific ways in our bodies.
Does that mean that fructose might have unique properties that could increase our diabetes risk?
Let’s take a look.
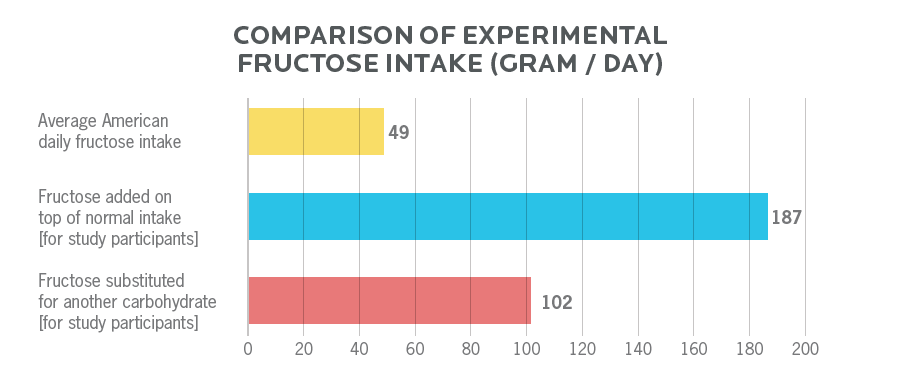
One meta-analysis looked at 64 substitution trials (in which fructose replaced another carbohydrate with no change in total calories), and 16 addition trials (where fructose was added to normal intake).
- In the trials where fructose was substituted for another carbohydrate, the average fructose intake was 102 g per day.
- In the trials where fructose was added on top of the participants’ normal intake, the average fructose intake was 187 g per day.
Compared to the average American fructose consumption of ~49 g per day, these are extraordinary intakes. To achieve those kinds of intakes would require up to 13 cups of ice cream, or consumption of 10 cans of soda.
Possible? Yes.
Daily norm? Sure hope not.
A recent review paper summed up the state of the evidence on fructose nicely, essentially stating:
The best-quality evidence to date does not support the theory that fructose intake directly causes cardiometabolic diseases.
The review added that fructose-containing sugars can lead to weight gain, along with increases in cardiometabolic risk factors and disease, but only if those fructose-laden foods provide excess calories.
Overall, research does suggest that a high intake of all sugar (including fructose) might slightly increase the risk of diabetes development by itself.
However, this research also indicates that most of this risk is due to the high sugar intake leading to excess calorie intake, and therefore increased body fat (which leads to inflammation, and ultimately insulin resistance).
An absolutely immense amount of research consistently and strongly indicates that the main causes of diabetes are:
- excess body fat,
- inadequate physical activity, and
- genetic predisposition.
On that last point, we know that diabetes risk, as well as risk of metabolic diseases and propensity to gain body fat, differs significantly by ethnic group or genetic subgroup. For instance, many groups of indigenous people are vastly more likely to struggle with these issues, as are people of African ancestry living in North America, or people of South Asian ancestry.
So your personal risk of these diseases also depends on where your ancestors came from, what genetic makeup they gave you, and/or how that genetic makeup interacts with your environment.
The bottom line here: Managing your sugar intake is just one small tool in your diabetes-fightin’ toolbox. However, far and away, the most useful tool is weight (and body fat) management, however you manage to accomplish it.
Question #4:
Does sugar cause cardiovascular disease?
The term “cardiometabolic disease” refers to a broad group of related diseases, like the Type 2 diabetes we mention above, along with other diseases related to the complex phenomenon of:
- metabolic disruption,
- changes in hormonal and cell signaling,
- inflammation, and
- an inability to regulate normal physiological processes (like DNA repair).
These diseases can appear in many organs or organ systems. When they hit the heart and/or circulatory system of blood vessels, we call them “cardiovascular disease”. They show up as things like heart attacks, strokes, clogged arteries, and so forth.
A heart attack, or heart disease, used to be a death sentence. With better treatment and new medications, people are surviving longer and living better with cardiovascular disease.
Over the past 50 years or so, deaths from heart disease have declined by over 60% despite sugar intake increasing by about 20 lbs per person per year over that time (and by more than 30 lbs per person per year at the 1999 peak intake).
Researchers estimate that about half of that 60% decrease might be from better medical care. The other half likely comes from reducing the risk factors, such as:
- lowering blood pressure
- smoking less
- lowering blood cholesterol levels
Of course, as we’ve seen, consuming more energy in the form of sugar can increase body fat. And, because of its chemically active nature, more body fat definitely increases cardiovascular disease risk.
So eating a lot of sugar can certainly play a role.
But cardiovascular disease, as with other metabolic diseases, is complex.
It’s not just one thing.
It’s all the things.
It’s how we live, how we work, how active we are, how stressed we are, what’s in our environment, and the various other factors that influence our health.
There are other factors besides sugar in metabolic disease.
Indeed, if we look at factors that we know for sure are related to the risk of metabolic disease, only about 3% of Americans uphold four essential healthy lifestyle behaviors consistently:
- Not smoking.
- Maintaining a healthy body weight.
- Eating 5 or more servings of fruits and vegetables per day.
- Being physically active at least 30 minutes a day 5 times a week at a moderate intensity.
On top of that, let’s consider two other known preventative methods for metabolic disease…
- Keeping stress levels moderate.
- Sleeping well, 7-9 hours per night, consistently.
…now we’re probably at 1% of Americans.
Once again, sugar intake is probably one piece of the puzzle. But it’s just one piece—and probably a very small one.
Question #5:
How much sugar is OK to eat?
Let’s get real here.
Sugar is not a health food.
It doesn’t nourish us.
It doesn’t add a lot of nutrient value: It doesn’t give us any vitamins, minerals, phytonutrients, antioxidants, fiber, or water.
Eating a lot of sugar doesn’t make our bodies better, stronger, healthier, or more functional.
Sugar doesn’t add value, certainly not when compared to other foods or macronutrients like protein or omega-3 fatty acids.
But biology is complex.
Diseases are complex too.
We can’t blame one chemical for all the health problems we have.
Good health is neither created nor destroyed by a single food.
Again, human beings are diverse.
We vary widely in all kinds of ways, including:
- How much carbohydrates we need to thrive or perform well.
- How well we digest, absorb, and use sugars, as well as how effectively and safely we store or dispose of the excess.
- How sugar affects our appetite, hunger, fullness, ability to stop eating it.
- How we feel about and behave around sugar.
- How sugar “spins our brain dials” and gives us a sense of reward.
So we can’t say that “X amount of sugar is always best for everyone, all the time” or that “People should never eat any sugar.” It just doesn’t work that way.
- Some people might choose to cut out sugar completely.
- Some people might try to micromanage their intake down to the gram.
- Some people can just roll with a general “eat less-processed foods” guideline, and be fine.
- Some people do find that a low-sugar, low-carb or even a ketogenic diet works for them. While others thrive on high-carb diets.
That said, being aware of your sugar intake is probably a good idea.
The 2015-2020 Dietary Guidelines for Americans recommends limiting sugar to 10% of your intake. So, for example, if you’re consuming 2000 calories per day, that would be approximately 200 calories from sugar, or 50 grams.
What does this all mean?
Let’s sum up what the science suggests:
- Sugars are basic biological molecules that our bodies use in many ways.
- Each person’s response to sugar (whether physiological or behavioral) will be a little different. This goes for carbohydrates in general too.
- Sugar is not a health food. But sugar alone doesn’t necessarily cause most chronic health problems like diabetes or cardiovascular diseases, which are multifactorial.
- Sugar is energy dense. If eaten in excess (like most foods), sugar can contribute to weight / fat gain.
- This weight / fat gain is probably mostly from the extra calories, not some special properties of sugars (or carbohydrates in general, or insulin).
- Some people find it hard to stop eating sugar / sweet foods. This may also contribute to weight / fat gain—again, because of the extra energy intake.
- We likely eat more sugar than we realize, since it’s hidden in so many food products.
Yet, after working with thousands of clients:
For most people, cutting out sugar completely, trying to abide by rigid rules, or basing dietary decisions on fear, probably isn’t sustainable or realistic.
That’s why, at Precision Nutrition, we prefer a more balanced approach.
What to do next:
Some tips from Precision Nutrition.
1. Recognize that health concerns are more complex than a single smoking gun.
The fitness and nutrition industry loves to say that one factor is responsible for everything (or that one magical food / workout / mantra will cure everything). It also loves to over-simplify and moralize (e.g. this is “bad”, this is “good”).
You don’t have to understand physiology to grasp the idea that things are complex.
There are many factors that go into good health, athletic performance, physical function, and wellbeing.
This means you should…
2. Begin with fundamental behaviors.
Sugar is one part in a much bigger puzzle.
Review this checklist and see how many of these fundamental behaviors you do well and consistently. That means every day, or most days:
- Don’t smoke.
- Keep your alcohol intake moderate.
- Eat slowly and mindfully.
- Eat enough lean protein.
- Eat 5+ servings of fruit and/or veggies per day, ideally colorful ones.
- Eat some healthy fats.
- Get some movement for at least 20-30 minutes a day.
- Get 7-9 hours of good-quality sleep every night.
- Reduce stress.
- Spend time with people you love, and/or who support you.
- Do things that are meaningful and purposeful to you.
These are all behaviors that we know for sure are health-promoting and disease-preventing.
3. Become aware of your overall energy balance.
Take a clear-headed look at how much food you’re eating for your body’s needs, and how much activity you’re doing.
Are you eating the right amount for your physiological requirements?
If you’re heavier or carrying more body fat than you’d prefer, you may need to adjust how much you are eating and/or exercising.
This may mean lowering your sugar intake, and/or it may mean eating a little less of other foods overall.
4. Become aware of what’s in your food.
Read labels. Sugar lives in processed foods, even foods you wouldn’t expect (like salad dressings or frozen dinners).
Better than reading labels, ask how you can eat more foods without labels. (Like fruits and veggies, beans and legumes, nuts and seeds, meats and seafood, etc.)
Transitioning to less-processed and less-sweetened versions of various foods is a simple way to lower your sugar intake and get the benefits of a better nutrient intake. Double win!
5. Maintain a healthy weight.
There is no single “healthy” weight. Your weight may be higher than average, or it may be within a “normal” range.
What is most important is that this weight is healthy for you (which you’ll know because all your indicators like blood work or athletic performance and recovery look good).
If you think you need to lose a little weight/fat to look, feel, and/or perform better, the good news is that you often don’t need to lose very much to see metabolic benefits.
You don’t have to be super-lean… and in fact, many people won’t benefit from trying to do that anyway.
6. Be mindful of your overall eating patterns, habits, and perspectives.
Consider…
- Are you eating slowly and mindfully? Can you stop when you’re satisfied?
- Are you using sugar-rich foods as a “treat”? How often?
- Do you feel “deprived” if you don’t “get” to have sugar?
- If you have a sugary food, can you stop eating it when you’ve had “enough”? Is there an “enough” with some foods?
- How does sugar fit into your life and overall habits? Is that working for you?
7. Keep it in perspective. Add “treats” in moderation.
Around here, we keep it real.
We like “treats”, “junk food” and tasty stuff just as much as anyone else, whether that’s a glass of wine, a bowl of ice cream, or a hot dog at the ball game.
We just keep the portions moderate and don’t have “treats” for breakfast, lunch, and dinner every day.
For most people, a little bit of sugar fits just fine into an overall healthy diet pattern.
If you’re looking for numbers, we suggest you shoot for including “treats” or other discretionary indulgences at 10-20% of your meals. If you eat 3 meals a day for a week, that means about 2-4 of those 21 meals might include something fun or “less nutritious”.
8. Ask yourself what works for you and what doesn’t.
If you struggle with sugar (for instance, if it makes you feel ill, or you feel like you can’t eat sweet foods in appropriate amounts), then it’s probably not a good food for YOU.
Try experimenting with lowering your sugar intake gradually (for instance, by making simple substitutions like drinking water or seltzer instead of soda), and see what happens.
Look for foods that you love, and that love you back—that make you feel good and perform well, that give you sustained and long-lasting energy, that keep your moods level, and that keep you feeling “normal” as an eater.
9. If you’re a coach, keep it real and positive.
Don’t scare your clients. Don’t lecture them. Don’t moralize.
Help them. Learn about them. Understand them.
Although research may say that on average low-carb is no more effective than other dietary strategies long-term, or that sugar by itself is not addictive, or any other innumerable statistics, your clients are real people. They are not averages.
Each individual’s preferred approach, unique circumstances, and personal experiences have to be carefully considered and taken into account when working together.
Go slowly, step by step. Make sure your client can actually do what needs to be done.
Fit the dietary strategy to the client, not the client to the dietary strategy.
10. Use data.
Track your health and physical performance indicators.
Schedule regular medical checkups.
Look at stuff like how you feel, how your mood is, how you sleep, how your bloodwork looks, how well you recover from workouts (and life in general), etc.
Follow the evidence. If everything looks stellar, keep doing whatever you’re doing
Worried you’re eating too much sugar? Wondering how much is safe to eat? Or whether it’s bad for you… no matter what? It’s time we took a clear-headed look at this topic. It’s time you heard the truth about sugar.